What is ECMO therapy?
Miscellaneous
This treatment option can give very sick patients a chance at survival
When more conventional forms of treatment don’t meet goals or help the patient progress forward in their healing and recovery, St. Joseph’s/Candler can provide extracorporeal membrane oxygenation therapy, or ECMO.
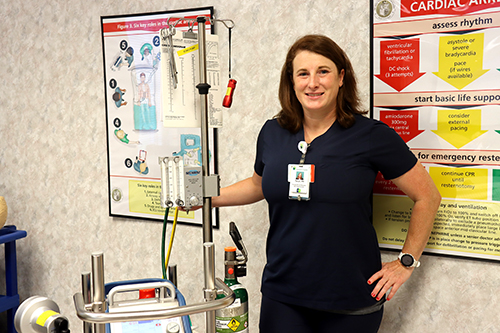
ECMO is a device that pulls the blood out of the body and allows gas exchange with oxygen and carbon dioxide before returning the oxygenated blood to the body, explains Tanya Coggins, clinical nurse educator for our coronary care unit (CCU) and cardiovascular intensive care unit (CVICU) at St. Joseph’s Hospital.
“It allows for the lungs to rest while the body’s other organs still get perfused with oxygenated blood,” Coggins says. “It’s not a cure but a supportive therapy.”
The ECMO machine used to look more like a washing machine and took up the whole room, but as improvements have been made it’s now hand-held and transportable, Coggins says. It sits on a cart and has two tubes that continuously cycle the patient’s own blood through the device and back to the patient. ECMO cycles an average rate of about four liters per minute, or 600 milliliters per second, Coggins says.
It is a complex therapy, so extra training for ECMO is provided to the nurses in CCU/CVICU, which is the only unit at St. Joseph’s/Candler to provide ECMO therapy. Nurses in both hospitals’ intensive care units are trained on preparing and advocating for patients if they need ECMO therapy, but all patients who need it will be transferred to CCU/CVICU.
Related Article: What to expect on our coronary care unit
So who may need this type of intensive therapy?

- As a modality to help bridge to a treatment or therapy when all other devices and treatment therapies have been utilized.
- For patients unable to oxygenate due to illnesses such as the flu, COVID, pneumonia or other viruses.
- Patients who are at high risk for cardiac surgery.
- Patients who are waiting on a transplant or waiting to be transferred to a hospital for a transplant procedure.
How long a patient is on an ECMO device varies from patient to patient. If it’s used for cardiac support, the patient may be on the machine a few hours or up to seven days. For lung treatment patients, the average time is up to three weeks, and for transplant patients, it could be months waiting for a transplant.
“I think ECMO is vital for this unit,” Coggins says. “With the closest transplant centers hours away, we can at least give patients that accelerated care and buy them time to make a decision or find out if they are a transplant candidate.”
St. Joseph’s/Candler has offered ECMO therapy since 2014. We are one of only a few health systems in the region to offer the modality. Coggins says many patients from regional hospitals will transfer to St. Joseph’s Hospital to be put on ECMO.
“It helps give the patient time for their body to fight against whatever virus they maybe experiencing,” Coggins says. “It’s not permanent. It’s not a cure. It’s there to help buy time, to allow other treatment options to work or evaluate for a transplant or provide extra time for the family.”